Chronic Inflammatory Demyelinating Polyradiculoneuropathy
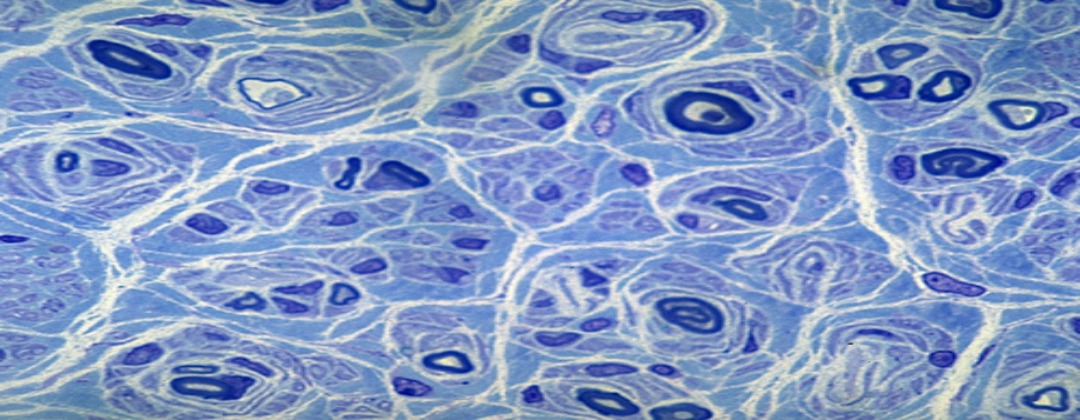
Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) is an autoimmune disorder, meaning the body attacks its own tissues. In CIDP, the myelin sheaths — the fatty covering on the fibers that insulate and protect your body’s nerves — are under attack.
Experts think that CIDP is related to the more commonly known disease Guillain-Barre syndrome (GBS). But while GBS is generally considered more of an acute, or short-term, disease, CIDP is considered a chronic, or long-term, disease. It is also rarer than Guillain-Barre syndrome.
CIDP is usually classified by these three types:
-
Progressive. The disease continues to worsen over time
-
Recurrent. Episodes of symptoms that stop and start
-
Monophasic. One bout of the disease that lasts one to three years and doesn’t recur
Symptoms
Regardless of the type of CIDP you may have, symptoms are usually the same:
-
Tingling in your arms and legs
-
Gradual weakening of your arms and legs
-
Loss of reflexes
-
Loss of balance and your ability to walk
-
Loss of feeling in your arms and legs, which often starts with your inability to feel a pin prick
Who’s at risk
CIDP is a rare disease. The number of Americans affected is somewhere between 1.5 and 3.6 per million. Only 40,000 people exhibit symptoms at any one time. Though the disease can occur in anyone, people in their 50s and 60s seem more likely to develop CIDP than other age groups. Men are twice as likely as women to get the disease.
Diagnosis
Because of the rarity of CIDP, it’s often difficult for doctors to correctly diagnose the disease, at least at first. Doctors can confuse its symptoms with those of GBS, because of the similarity between the two diseases. If symptoms last longer than eight weeks, your doctor may suspect CIDP.
A specialist will perform an exam and possibly conduct blood and urine tests. He or she may conduct a nerve conduction study to look for myelin damage in peripheral nerves. This test is sometimes called an electromyogram. It involves using low electrical currents to test nerve function and response. To help diagnose CIDP, you may need a lumbar puncture. In this procedure, a specialist inserts a small needle in your back and draws a sample of your cerebrospinal fluid. This is the fluid that surrounds your spinal cord. The procedure helps doctors detect elevated levels of certain proteins related to the disease.
Treatment
Once you doctor diagnoses CIDP, treatment is often effective. Some studies show that up to 80 percent of people respond well to therapy. Because it is an autoimmune disorder, the disease is treated with medications that suppress your immune response. Your medical team tailors your treatment to you and closely monitors your progress. Treatments for CIDP include immunosuppressive drugs, steroids, intravenous immunoglobulin, and plasma exchange.
Complications
If you do not seek treatment for CIDP, your symptoms will progress over the course of several years. These will range from sensory symptoms, such as tingling and numbness, to motor sensations, like complete loss of feeling and loss of balance. Without treatment, 30 percent of those with CIDP can end up needing a wheelchair. Early diagnosis and treatment are extremely important.
When to call the doctor
If you notice any CIDP symptoms, talk with your health care provider.